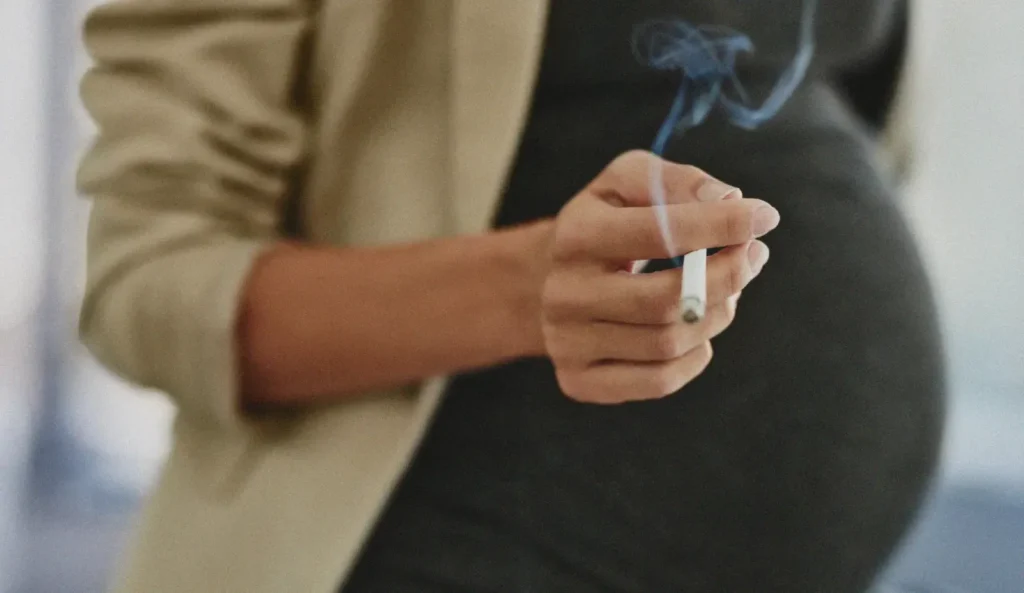
Pregnancy and smoking: general information
World No Tobacco Day, organized by the WHO, takes place on May 31st of each year. During the 2011 edition, the French government announced an increase in the reimbursement of smoking cessation treatments from 50 to 150 euros per year for pregnant women. Since January 1, 2019, nicotine replacement therapy has been reimbursed at 65% by the French Health Insurance.
The majority of young smokers say they will quit when they “have a baby.” However, 35% of women are still smokers at the beginning of their pregnancy. Among these, many want to quit. However, two-thirds of them are still smoking on the day they give birth.
Indeed, according to the website of the Ministry of Labor, Health and Solidarity, 17.8% of pregnant women in France still smoke during the third trimester of their pregnancy. This is the highest rate in Europe, despite the health risks to pregnancy and the health of the child.
The risks to the unborn baby are now known and make this particular form of smoking a public health issue.
Impacts of smoking on pregnancy
Smoking is an addiction to products made from tobacco leaves. The most addictive element in these products is nicotine, the main ingredient in cigarettes, for example.
Cigarette smoke contains 4,000 chemical substances, 60 of which are classified as carcinogenic by the International Committee for Research on Cancer. These substances are, in addition to nicotine:
- tars;
- irritating substances;
- carbon monoxide;
- acetaldehyde;
- anabasine;
- ammonia;
- benzene;
- lead;
- etc.
All of these substances have recognized harmful effects on pregnant women and their fetuses. Indeed, it has now been shown that smoking during pregnancy and breastfeeding leads to:
- intrauterine growth retardation due to the passage of carbon monoxide into the fetus’s blood;
- a reduction in birth weight ( hypotrophy );
- a risk of premature delivery;
- birth defects: Smoking may increase the risk of birth defects, such as facial, heart, and lung defects;
- placental complications: Nicotine has a vasoconstrictor effect on the arteries of the placenta and on the umbilical artery, which makes blood circulation less good.
- an increase in lower respiratory infections and ear infections in the unborn child;
- an increase in the rate of sudden infant death;
- a low-lying placenta;
- a change in the taste of milk if the child is breastfed;
- a risk of being overweight in adolescence
Good to know : Making pregnant women feel guilty by reminding them of their “irresponsibility” and continually listing the risks they pose to their fetus rarely helps with the cessation process. The motivation to quit should primarily come from the smoker herself.
Strategies to Quit Smoking
It’s never too late to quit smoking during pregnancy, even if you’re already well into your pregnancy. Quitting smoking, even for a short time, can significantly improve the health of both mother and baby.
Preliminary assessment
As with any smoker, optimal care for a pregnant woman who smokes begins with questioning about:
- his health history;
- his personal and family background;
- his socio-professional environment;
- his smoking history;
- any co-addictions (alcohol, cannabis, etc.).
This interrogation assessment is generally followed by:
- of a complete clinical examination;
- of an assessment of dependence by the Fagerström test ;
- An assessment of smoking behavior using the Horn test.
- an assessment of the smoker’s motivation to quit, via various tests of choice ( Richmond test, Demaria, Grimaldi, and Lagrue test ).
Weaning methods
There are many supports available to pregnant women who want to quit smoking, including:
- psychological support provided by a psychologist or psychiatrist;
- Cognitive behavioral therapies (CBT): These therapies can help identify and change thoughts and behaviors that contribute to smoking.
- pharmacological management: prescription of nicotine substitutes such as NRT. It is recommended to use NRT in combination with a psychological and/or behavioral approach.
- Consultation with a tobacco specialist: he can provide individualized support and advice to quit smoking.
Good to know : bupropion LP and varenicline are contraindicated in pregnant women.
Resources and Support
For some women, planning to have children is often a good motivation to quit smoking. For those who are unable to do so, there are several methods and resources to help with the process:
- Specialized consultations to help with quitting: Pregnant women who smoke can contact their health insurance fund to obtain a list of support structures.
- The Tabac info service listening line (3989);
- The Tabac Info Service website.
- The Tabac info service web application, which offers 100% personalized coaching.
- local anti-smoking associations;
- healthcare professionals (doctor, midwife, PMI).
Pregnant women can either:
- quit smoking alone (using nicotine replacement therapy);
- quit smoking as a group, thanks in particular to the #MoisSansTabac challenge, which comes back every year in November;
- Call on health professionals.
Pregnancy is a period that requires regular consultation with medical professionals. It is therefore a special and privileged time for health professionals to provide information on the consequences of smoking in pregnant women and on passive smoking.
Good to know: Women who are still smoking on the day they give birth aren’t irresponsible, but rather powerless over their tobacco addiction. It’s essential to support them in their cessation, not judge them